The Public Health Emergency is Ending
In January 2020, the U.S. Department of Health and Human Services (HHS) declared a Public Health Emergency (PHE) in response to the outbreak of COVID-19. Congress subsequently passed legislation that guaranteed anyone enrolled in Health First Colorado (Colorado’s Medicaid program) could keep their health coverage during the PHE. However, once the PHE has concluded, all individuals currently enrolled in Medicaid will need to go through the redetermination process to ensure that they still qualify.
President Biden has announced that the Public Health Emergency will end on May 11, 2023. However, the Department gave direction to States requiring them to start redetermining Medicaid eligibility by April 1, 2023. States will have up to 14 months to redetermine eligibility.
The Colorado Department of Health Care Policy and Financing, otherwise known as Health First Colorado, will be contacting all Medicaid clients by mail starting in March 2023 to inform them of restarting the revalidation process. The first redeterminations will be due by May 2023.
What This Means for You
This renewal process will need to be completed by all individuals currently receiving Medicaid. It is anticipated that 315,000 recipients in Colorado will no longer be eligible after the redetermination process is complete. However, a majority of upcoming denials are anticipated to be caused by not completing the required steps on time. These preventable instances can be avoided by taking the necessary steps as outlined below.
How can I prepare?
There are four crucial steps that need to be completed to successfully submit redetermination paperwork. These redetermination packets are time sensitive, and you must return all the requested information by the deadline date in the letter you will receive from the state.
To be prepared, we encourage all PASCO caregivers to take the following steps:

1. Confirm and/or update your contact information
This step is crucial to ensure that you are receiving your Medicaid renewal paperwork at the correct location. This first step will allow all remaining processes to occur.
Updating your address, phone number, and email is quick and easy. You can update your information in one of these ways:
-
- Visit Colorado.gov/PEAK. If you don’t have a PEAK account, you can create one at Colorado.gov/PEAK.
- Use the Health First Colorado app on your phone. This free app is for Health First Colorado and CHP+ members. Download it for free in the Google Play or Apple App stores.
- CHP+ members can call 800-359-1991 (State Relay: 711). Help is available in multiple languages.
- Contact your County Department of Human Services or Social Services to change your contact information. You can find your County office at: https://cdhs.colorado.gov/our-partners/counties/contact-your-county-human-services-department
- Contact PASCO if you need assistance with this process.

2. Check your mail for your renewal letter
You will receive a letter and an email informing you of your renewal date. This date is crucial, as it indicates when you can anticipate when you will receive your redetermination packet and begin the renewal process.
PLEASE NOTE: Some individuals will be automatically renewed based on information we have for them from other data sources. This means that some members will not receive a renewal packet, but rather receive a “notice of action” letter that lets them know they are still eligible for coverage.
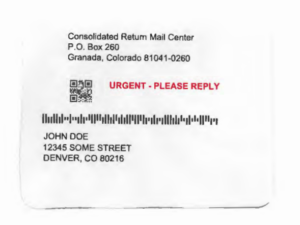
As seen in the example below, the letter will be sent from “Consolidated Return Mail Center” with URGENT – PLEASE REPLY written in red.
3. Receive and sign the redetermination packet
Members will receive a renewal packet approximately 70 calendar days before their renewal deadline to allow time for completion. Your renewal date can be reviewed at CO.gov/PEAK. Some individuals will be required to provide additional information, like changes in income, care needs, and more. Even if no additional information is needed on your part to complete the process, this packet MUST be signed and returned by the deadline listed.

4. Return signed packet
This packet must be signed and returned on time. This can be completed via the following:
-
- Online at: CO.gov/PEAK
- Through the Health First Colorado App
- By mail, fax, or bring the completed signature page and updated renewal form pages to the local county office
BE ALERT: Medicaid Text and Phone Scams
Scammers are targeting Health First Colorado (Colorado’s Medicaid program) and Child Health Plan Plus (CHP+) members through text messages and phone calls. They are telling members they must pay to keep or renew their health coverage.
Health Care Policy & Financing (HCPF) never asks members or applicants for money, bank account or credit card information, social security numbers, or any other financial information through text or over the phone. Please help us spread the word and report any suspected scam activity to the Attorney General Consumer Protection Unit.
Me and my family have Medicai due to my low income. Do I have to sign those documents that you mention?
Hi Guadalupe! Yes – all individuals receiving Medicaid will have to go through the renewal process. The letter you receive in the mail will let you know of any additional action or information you may need to provide to complete the process.
I didn’t get any letter from Medicaid, and it is not in my Peak Colorado account either, what should i do?
Hi Raquel,
You will receive your letter about 70 days prior to when your loved one is set to renew coverage. This can be at any point in the next 12 months – but you can check on that renewal date in the PEAK page.
Here is how to find that date: On the main navigation, choose “Manage my benefits” and then “Overview of health coverage benefits.” Then,
find renewal due dates for each household member under “Summary of health coverage benefits.
I hope this helps!