What is Behavioral Therapy or ABA (Applied Behavior Analysis)?
“Applied Behavior Analysis is the science in which procedures derived from the principles of behavior are systematically applied to improve socially significant behavior to a meaningful degree and to demonstrate experimentally that the procedures employed were responsible for the improvement in behavior.” (Cooper et al., 1987, pp. 14)
How is Behavior Defined in ABA?
Behavior: “Everything that people do, including how they move and what they say, think and feel.” (Cooper et al., 2007, pp. 25) Behavior must be OBSERVABLE by others and MEASURABLE for data collection purposes.
How is Behavior Observed and Evaluated?
- Environment
- Context
- Value
It is important to observe how the environment affects behavior and to explore the context in which the behavior occurs. Once these observations are made it is paramount to understand the value of this behavior and its impact on the individual, family, and community.
The evaluation process incorporates the principles and procedures of behavior analysis to ensure that the client’s health, independence, and quality of life are improved. Evaluations are consistent and ongoing with objective assessment and data analysis informing clinical decision-making.


How to Identify Behavioral Challenges from an ABA Perspective?
- The social significance of behavior
- Must be meaningful for the client, not the provider
- The social significance of the intervention
- Intervention must be least intrusive yet effective
- Socially valid intervention
- Intervention should promote & protect the dignity of the individual
- Ethical application of the science
- Informed consent
- Incorporation of client’s/legal guardian’s choice & priority
- Measurable
- Data collection to ensure progress
- Visual representation & analysis of data
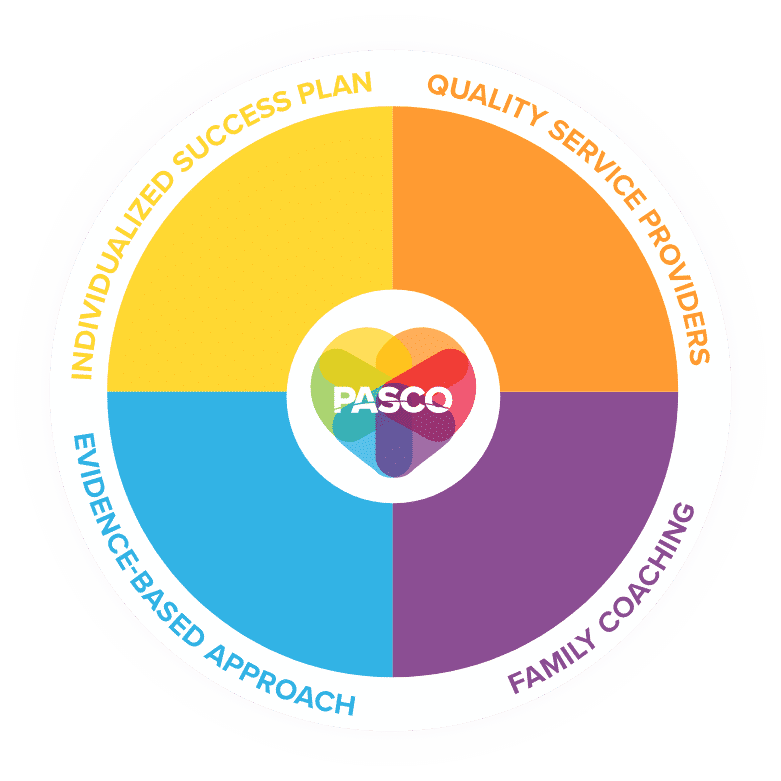
What to Look for in a Provider of Behavioral Therapy / ABA?
- Individualized Success Plans
- No two individuals are alike and the ABA provider should tailor each success plan to the individual in order to achieve positive change.
- Quality Service Providers
- Only Board Certified Behavior Analysts and Registered Behavior Technicians should provide services.
- Evidence-Based Approach
- The field of ABA has developed many techniques for increasing useful behaviors and reducing those behaviors that may cause harm or interfere with learning.
- Family Coaching
- Providers should coach the individual’s family members on strategies to promote positive behaviors.
How Does the Process of Obtaining Behavioral Therapy / ABA Services Work?

Intake
The process begins with an initial phone call with the family or case manager to gather basic information about the individual seeking services. This includes ensuring that the funding source covers services, discuss availability, and to discuss behaviors of concern or areas of needed skill acquisition.
An intake packet is sent out to the family consisting of basic information, client rights, consent for treatment documentation, and authorizations to release and exchange confidential info.
Assessment
A Board Certified Behavior Analyst or a Master’s level RBT will meet with the family to discuss behaviors of concern, skill acquisition areas of concern, and goals for treatment. The provider will observe and take notes on the behaviors as they occur in the home setting. The provider will initially conduct a Functional Behavior Assessment to determine the intent of the behavior. The assessment is used to find an alternate, more socially significant behavior to teach that meets the same function in a more appropriate way. Families will fill out at a Vineland assessment which evaluates the areas in which the individual requires intervention such as communication, motor skill development (for individuals younger than 6), daily living skills, socialization, and maladaptive behavior.
Treatment plan
The provider will create a treatment plan with both short and long-term goals and will review them with the family. Once the family has signed the treatment plan it will be submitted along with the assessment, a letter of medical necessity for ABA from their doctor, and a diagnostic report.
Authorization
The funding source will give authorization or denial of services.
If a denial is given, the agency may appeal by providing additional information. If the denial is due to the services not being a covered benefit, the family may have to seek services through another in-network agency that is covered or seek an alternate funding source.
Regular Services Begin
After receiving authorization the agency will be able to provide regular daily/weekly services.
Daily services are provided by a Registered Behavior Technician who is trained and supervised by the BCBA. The RBT will work regularly with the family and will be supervised by the BCBA at least 5% of the time. At PASCO, we aim for 20% supervision. Supervision ensures that the services provided are following the treatment plan and are working towards meeting the goals outlined. The RBT will record data throughout each session which the BCBA will graph to evaluate the success of the interventions and to determine if new interventions need to be applied.
Colorado Medicaid Requirements
Colorado Medicaid is a part of a federal guideline from state to state to provide medical care for those in low income brackets.
In order to participate in Colorado’s medicaid system you must be below a specific income limit:
Household Size / Income
1: $16,612
2: $22,491
3: $28,369
4: $34,248
5: $40,127
6: $46,005
7: $51,884
8: $57,762
If you meet the above income requirements you are eligible to apply to the Colorado medicaid system which provides free or low-cost health coverage.
Usually this healthcare system is provided in the form of a health-care insurance marketplace. Many providers will list their health insurance under the marketplace and once eligible, you will be able to search through this marketplace and find the right insurance for you.
Many of these insurances are either free or drastically reduced in price. Many have various benefits such as no monthly premium, low deductibles, and so on.
This is a great option for families or individuals that are struggling to obtain health care due to a low income situation.
How to Access Behavioral Therapy Services?

Health First Colorado (Medicaid)
Behavioral Therapy Services are a covered benefit for all individuals with Medicaid coverage regardless of diagnosis.
However, if a family has primary insurance they would have to utilize their primary insurance first. Medicaid is the payer of last resort, therefore they would have to obtain a denial letter from the primary insurance stating that ABA services are not a covered benefit (only applicable to individuals not diagnosed with ASD or self-funded employer plans).
Medicaid will not accept denial letters due to an agency being out-of-network. The denial must state that ABA is not a covered benefit under their plan to be able to then go through Medicaid as the funding source.
Families can apply for the Medicaid Buy-In Program through their local Community Centered Board. Once approved, the individual has full Medicaid coverage including behavioral health benefits. Families can apply for the Child-Only Medicaid Buy-In. There is a monthly premium based on income associated with the buy-in program. For a list of qualifying disabilities please visit the Social Security Listing of Impairments.

Private Insurance
Beginning in July 2010, Colorado mandated that all employer-provided health insurance regulated by the state of Colorado cover Applied Behavior Analysis services for individuals diagnosed with Autism Spectrum Disorder. This mandate applies to children under the age of 19.
What does this mean for families?
If you have an employer-provided primary insurance you will need to go through an agency that is considered in-network if the individual seeking services has an ASD diagnosis. It is mandated that insurance companies cover these services but only through their contracted agencies.
If a family chooses to go through an out-of-network agency and they have secondary insurance such as Medicaid, Medicaid may not cover additional expenses and families will have to pay the out-of-pocket cost.
If the individual does not have an ASD diagnosis, families may then go through their secondary insurance if they have one (often Medicaid). The family will have to obtain a letter of denial of services from their primary insurance to be able to go through Medicaid for services. If the secondary insurance is Medicaid, Medicaid becomes the payor of last resort and the family will not accrue costs related to ABA services.
Private Pay
Most agencies offer private pay. Contact them directly to see what their rates are.
Tips and Tricks
- Reach out to agencies on your own
- Get on multiple waitlists
- Doctors and case managers can send referrals
- Daytime availability can shorten the wait time
- Contact your local CCB for extra support
- Be patient
- Stay positive
Families can reach out to companies themselves. It is beneficial to get on multiple waitlists at one time as many agencies currently have a wait for services in the Denver Metro Area.
A family cannot receive behavioral therapy services from multiple agencies at one time. However, they can get on a waitlist while receiving services if their current provider is not the right fit.
A family receiving services who would like to switch to a new agency can keep their current services going until the new agency applies for authorization from their insurance company. This is the best way to make sure the lapse in services is minimal. For Medicaid, the new agency submits a change of provider form with their treatment plan and request for authorization. With many other insurances, the family needs to call the insurance company and let them know that they would like to switch to the new agency.
Doctors/case managers can refer to an agency. Often times Doctors and case managers will send referrals via fax to multiple agencies to get services started for their patients and to ensure that their patients get on several waiting lists.